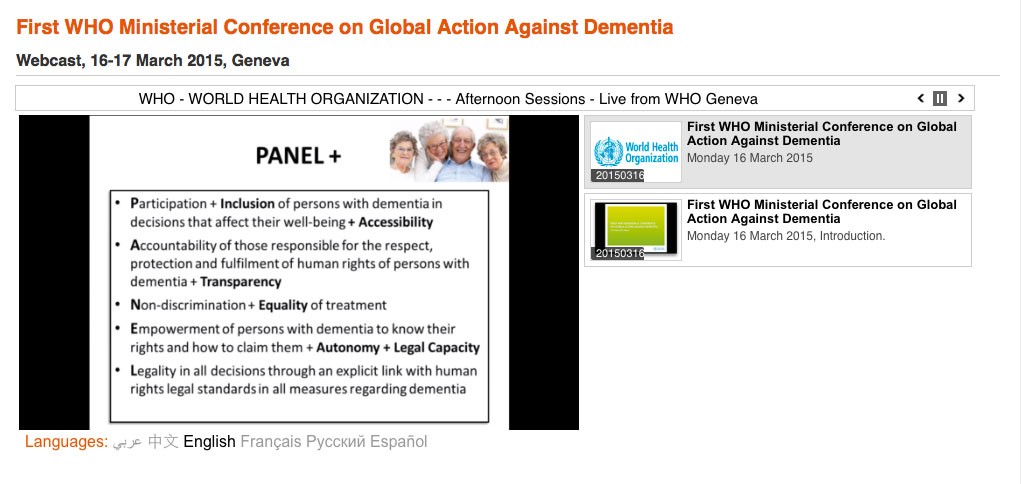
“Urgent” and “call for action” have become the potent memes in messaging radical transformative change. Hence the title of the statement about the #globaldementia event, held earlier this week in Geneva, came as no surprise to me. What did genuinely come as a surprise was how accommodating both WHO and the Alzheimer’s Disease International were to the views of people with dementia there.
This was the public image; rather reminiscent of GCHQ, an omniscient and omnipotent body talking to each other. And indeed I found the communication between officials between different countries useful, even some still clung onto the deeply stigmatising language such as ‘horrific’ and ‘devastating’.

The word though ‘urgent’ does merit some scrutiny. It implies that time is running out – and indeed Hillary Doxford, the representative of the World Dementia Council living well with dementia, explained that “time is the currency of people living with dementia”. Hillary herself explained how she was only given a finite length of time to live, according to her initial disclosure diagnosis. And this is not the first time that I have heard this issue being totally mishandled. The actual truth is that it can be very difficult to predict how long a person will live, and actually imparting a diagnosis of dementia should not bring that person any closer to their time of death. In fact, ideally, we want to be able to get to the stage where most people, after a diagnosis of dementia, are able to ‘live better with dementia'; and indeed initial evidence appears to support the notion that active social networking or even diet may have a beneficial effect. But Kate Swaffer brought out a point which I do feel is urgent; that high quality research into care and living better with dementia needs to have parity as that sort of research which ultimately yield a ‘cure’. The ‘experts’ this week had enormous difficulty in identifying what a cure for dementia might look like, and this is not surprising given that there are about a hundred different types of dementia.
We didn’t hear much from caregivers themselves at the conference, which is not unexpected given what a full time job caregiving is. The “call for action” this time around. “Call for action” has become the call for arms for charities campaigning on dementia, but it is becoming increasingly clear that self-generating social movements campaigning for a change in how dementia is perceived by others is gathering considerably more momentum than the ‘dementia friendly communities’ construct. ‘Dementia friendly communities’ should not be underestimated for reframing aspects of communities around the needs of people in society with dementia to lead fulfilling independent lives, but it remains dangerously close to a “does he take sugar?” modus operandi. Even the “no decision about us without us” mantra assumes division of “them” against “us” – which led me to do my own personal #globaldementia pledge this time around.

I am looking forward to participating in an event hosted by the Mental Health Foundation on 26 March 2015 entitled, “Rights, dementia and the social model of disability: a new direction for policy and practice?” I must admit that I was expecting to be somewhat at odds with this report, but I found it spot on. I’d therefore like to extend my personal thanks to Gráinne McGettrick, members of the project Advisory Group, 26 March speakers and participants, especially people living with dementia.
The document is very much in keeping with chapter 13 of my book “Living better with dementia: Good practice and innovation for the future”, with three forewords having been written by Kate Swaffer, Co-Chair of the Dementia Alliance International, a ‘peak body’ of people living with dementia, Beth Britton, celebrated blogger and campaigner, and Chris Roberts, living well with dementia. The narrative of my book is ambitious; it basically puts people living with dementia, with an aspiration to live better, ‘in the driving seat’, and argues for a rôle for an individual who has received a diagnosis, a member of family or friend, and professional to take part in an extended network to help to deliver a personalised care plan. In chapter 13, I found myself confronting the rather individualistic approach of human rights, being reconciled with the ‘dementia friendly communities’ policy currently in vogue worldwide.
For me the Mental Health Foundation report throws up a number of critical policy issues which will need to be confronted sooner or later. I suggest sooner; perhaps even I suggest ‘urgently’ with a similar ‘call to action’?
The issues for me are as follows.
1. Definition of dementia under English law
The guidance for the Equality Act (2010) helpfully includes dementia as a disability. The case law, I feel, is more helpful than the statute law.
For the law, the link between ‘disability’ and ‘impairment’ is a key one Section 6(1) Equality Act [2010] states that a person (P) has a disability if P has a physical or mental impairment, and the impairment has a substantial and long term effect on P’s ability to carry out day to day activities.
In essence, the claimant must therefore show that there is an impairmen, the impairment has an adverse effect, the adverse effect is substantial, and the effect is long term.
Not all of the points have to be proved, and it has generally been accepted that claimants living with cancer, multiple sclerosis, or HIV/AIDS will have no problem in fulfilling this statutory definition. The legal issue is how a medical condition affects a person ((e.g. mobility, manual dexterity, co-ordination, continence, ability to lift/carry, speech, hearing, eyesight, memory, ability to learn, perception of risk or physical danger).
The medical model requires the clear identification of deficits; whereas the social model, one which people themselves with dementia tend to prefer, looks at what people can do rather than what they cannot do. Arguably, attending a medical ‘check up’ which emphasises what you cannot do now compared to before, or brain shrinkage on your MRI scan, can be very demoralising and not particularly constructive for a person living his or her life.
How the impairment is caused is irrelevant in English law, and we know this from Power v Panasonic UK Ltd [2003] IRLR 151, a case decided under the Disability Discrimination Act. There are possibly as many as hundred different types of dementia, and they all present with different ways, although it is certain that no two people living with dementia present the same. This calls into sharp focus of questioning what the point of the label is – such as the diagnostic category of dementia. In ‘diffuse lewy body type’ of dementia, certain medications are best avoided. Whereas dementia of the Alzheimer type typically is best characterised by early difficulties in learning and memory and spatial navigation, semantic dementia is best characterised by loss of specific types of knowledge, posterior cortical atrophy is best described as loss of higher visual processing early on, and behavioural variant frontotemporal dementia is most often characterised by an insidious change in personality and behaviour in the absence of cognitive deficits early on observed by others.
2. The enforceability of the law (access to justice)
Having an emphasis on the law is great to bolster that this a serious issue, rather than the more namby pamby softly softly approach of ‘dementia friendliness’. However, the usual criticisms of using a legal approach in my opinion apply; adherence to the law without a genuine change in cultural attitudes, a possible ‘race to the bottom’ with more enthusiasm about compliance than outcomes-focused regulation, or a sheer lack of enforceability due to drastic cuts in legal aid provision. In England, there has been quite savage cuts here consequent upon the Legal Aid and Sentencing and Punishment of Offenders Act (2012), which some rightly view as a demolition of the ‘welfare state’. One could and should argue, perhaps, that access to justice should be a necessary and critical part of a dementia friendly community?
3. The lack of cultural diversity considerations
The rights based approach is technically worthy of the same criticism as ‘dementia friendly communities’ in that in the drive to universal concrete individual rights there is little consideration of the cultural background of the person living with dementia (e.g. BAME communities, LBGT communities). But human rights by their nature are supposed to have a non-negotiable, inalienable fair about them, a universality which can be relied upon, so this may in fact be an advantage rather than a criticism. However, it could be argued that ‘dementia friendly communities’ offers a much more culturally-sensitive tool than rights-based approaches (see for example Dementia Friendly Gurudwaras).
4. Are rights and capacity connected?
The recent R v Cheshire/Chester case has brought to the fore the precise inalienability of human rights, which cover a mass of issues such as liberty, even if a person is legally without capacity. There is a broad consensus that a human person should not lose his or her human rights if he or she loses capacity, but this prerequisites a robust definition of capacity, which many feel we have simply not arrived in the current English jurisdiction (nor a consensus on the best way to implement the Mental Capacity Act (2005)).
5. Institutional vs ‘successful living’
Across the last few decades there has been a general move away of institutionalising people with mental health conditions including learning difficulties and dementia. There is nonetheless a tension which does interface with the ‘rights based’ approach and disability activism, in that people who are not able to live alone should not be deemed as ‘failures’ of policy.
6. Does the United Nations Convention of Rights for People with Disabilities inform on what might constitute a dementia friendly community? (e.g. enjoyment of sport)
The legal definitions under the United Nations Convention for Persons with Disabilities, as pertaining to dementia, are indeed interesting, as they refer to specific things such as enjoyment of sport. Of course, prescribing such a list lays the Convention to the attack of “expressio unius est exclusio alterius“, that only things specified n the list are worthy of consideration.
But they do potentially offer the basis of minimum legal standards for a dementia friendly community which could even be legally enforceable (in theory), such as article 30 (participation in cultural life, recreation, leisure and sport). Actually, I am quite interested in article 29 (participation in political and public life), which emphasises that the same democratic principles should apply for people with dementia. There was in fact a clear violation here, as the current nominee for the World Dementia Council, living well with dementia, was not democratically elected.
7. Implications for needs assessment under the Care Act (2014) in the English jurisdiction
The phenomenon that some people with dementia “have good days” and “have bad days” is well known not least to people with dementia and caregivers themselves. In certain types of dementia, such as diffuse Lewy body dementia, it is not unusual for cognitive performance to be ‘fluctuating’. The traditional description of ‘multi-infarct dementia’ (or ‘post stroke dementia’) has been of a ‘stepwise’ progression, although many have queried the correctness of this term.
Whatever the precise details, it is generally accepted that the needs of a person with dementia will change, not least because dementia, whatever the precise nosological definition, is considered to be progressive (unless the symptoms of dementia present from causes other than dementia or the dementia is ‘reversible’ e.g. plasma exchange for paraneoplastic dementia). This poses a critical question as to how rights are related, if at all, to the fluctuating symptoms of dementia? This logistically poses an issue of how often needs should be re-asssessed and how such ‘results’ are interpreted by professionals. Ideally, the benefits system linked to the Care Act (2014) regulations needs to be responsive to the care needs of any individual with dementia at any particular place and at any particular time. This certainly warrants careful scrutiny.
8. Shift from a medicalisation to a social model (rôle models, development of a cure, training of workforce)
This is of course is THE big one in England, requiring a huge radical transformative change in England, combining health and care.
This requires breaking down organisational silos, different funding schemes, different power structures, different workforce requirements, different cultural attitudes, the breaking down of barriers of information transfer, a more collaborative or distributive style of leadership, better coordination between different forms of care and health provision, the double declutching from a fragmented illness repair service to a national health service. The change required is enormous.
I have always believed that political leaders or CEOs of big charities do not hold the key to bringing out ‘urgent change’. And here you really have to define what change one is trying to bring about. Even the mantra “care for today, cure for tomorrow” has brought about division, as people have asked, “why not care for tomorrow as well?” Kate Swaffer, Co-Chair of the Dementia Alliance International, has warned that there is no imminent cure in the pipeline, so there is a genuine issue of expectation management. How are even the most altruistic of the 45 million people living globally with dementia supposed to get excited about a cure or Big Data advances in dementia for 2025?
Very difficult, if you’re being honest.
I believe rôle models, of people living well with dementia, such as Ken Howard, Kate Swaffer, Chris Roberts, Mick Carmody or Helga Rohra, hold the key here. They are THE authentic voice – to tell the organisers of the health and care services what is urgently needed from them, e.g. not 15 minute disclosures of diagnoses in the absence of loved ones with reference to an information pack in a busy clinic.
9. The power of the media
For all the efforts of destigmatising dementia, it is helpful if you have leaders in WHO or political Ministers of State calling “dementia” incessantly “horrific” and “devestating”. Nobody of course is asking for the negative aspects to be airbrushed out, but all most people want is some form of balance rather than ‘shock doctrine’ tactics. The stronghold of the media is not inconsiderable, especially if people with dementia are themselves to give birth themselves to a social movement, but here the tools of the new media, such as Facebook or Twitter, might help. One suspects that principal media outlets should be given much more stringent guidance on what is acceptable, and what isn’t.
10. Effective rehabilitation
Kate Swaffer herself noticed that ‘rehabilitation’ was noticeably absent from many if not all discussions. Why? Kate raised the point that if she had been given guidance on how to adjust to her diagnosis, on what she could do rather than what she could not do, she might have been able to carry on paid employment. Many people with dementia do not wish to take their employers to court over unfair dismissal, as that is a sure fire way to bring about a break down in employer-employee relations. That is an example where implementation of legal rights might bring about more damage than good. For many having received a diagnosis of dementia, effective engagement with the society and community is more beneficial than a lump sum payment from the employer, as we keep on being told in policy (because it is true) that marked loneliness often accompanies the diagnosis of dementia in all jurisdictions.
11. What is the end point? Equality versus diversity.
There is a sense that we do not actually know what the end point is for anything. We don’t even know what the end point for the cure for 2015 is, as we don’t have a coherent explanation of that despite numerous requests. Kate Swaffer suggested that a cure which gave somebody a protracted slow death might not be ideal either. And the “dementia friendly communities” policy is fixated on equality, not diversity, which means that even if both rights-based approaches and dementia friendly communities were implemented to the hilt across all jurisdictions to the hilt the policies would clearly not satisfy everybody because of individual differences in diagnosis and service provision.
12. Are the services in place which do not inadvertently encourage division?
Even the most professional professional this week confused dementia with a condition of ‘old age’. I have had this dispute with Kate Swaffer. In fact, we both agree. Many old people live with dementia. As you get older, your risk of getting dementia increases. But there are many younger people with dementia too. We haven’t reached a point yet where points of service provision are not ageist, and therefore immune from judicial review. How far do you take rights? I’ve asked Chris Roberts whether he feels that old people’s homes are appropriate for younger people with dementia, and Chris reliably tells me that he has not intrinsic difficulty into going into a home with older people as he loves meeting people (also telling me that the difference between 45 and 55 should not be given greater attention than the difference between 65 and 75).
13. Is involvement of charity a good thing? (Problems to do with corporate and regulatory capture; does involvement of “charity” inadvertently reinforce a ‘victimhood’ nature of living with dementia?)
The system is clearly geared up to reinforce the medical model; you can see the way possible cures for dementia are promoted by certain corporate-like charities; and this is reinforced by the regulator such as NICE setting rigid guidelines for such interventions (such as cholinesterase inhibitors) with less attention to say the potential of an iPod to improve the quality of life of a person with dementia through ‘musical therapy’. The cost of distributing iPods may be more ‘cost effective’ value-wise for improving quality of life of people living with dementia than medications which do not, for most, slow down progression nor have a beneficial effect of symptoms further to a very limited time window for some? Surely this is the sort of discussion we need to be having, as well as the ones we saw at #globaldementia? The time may have to come where large charities are recognised more as being as the problem than the solution, particularly if they appear to dismiss calls for a national network of clinical nursing specialists in dementia.
My somewhat reluctant conclusion is that rights-based approaches put people with dementias on a much firmer footing, and this cannot be a bad thing. However, my concern with this approach is that whilst right-based approaches appear fine in theory how they are actually implemented in real life which provide the acid test.
The national minimum wage sounds great, but…
Furthermore, one wonders whether the notion of living better with dementia rests easily with the concept of ‘victimhood’ which can inadvertently encroach on work.
Take for example, this recent section from an article from Norman McNamara’s Kickstarter to make a documentary about him and his initiatives:
“He added: “The Purple Angel Dementia Awareness Campaign has now become global and is being embraced by all four corners of the world.
“People who matter have come together for one cause – to help those less fortunate than themselves.”
It is unclear to what extent certain people with dementia are happy with this ‘victim status’ portrayed by others?