Full details of this conference are here.
Rosa Kornfeld-Matte (Independent Expert on the enjoyment of all human rights by older persons, mandated by UN Human Rights Council) was asked to speak.
This is a subject which interests me as I have been invited to an expert panel session at the Mental Health Foundation later this month on the subject of dementia as a disability.
Mark Pearson also spoke from the OECD on organising dementia care and services.
Pearson rightly in my opinion drew attention to the notion that people living with dementia do suffer from poor quality services.
More than half of people are not diagnosed as having dementia internationally, Pearson argues. But this is to ignore the considerable harm and distress in labelling someone as having a dementia diagnosis when he or she doesn’t.
But the subsequent statistics from Pearson are meritorious. A third of home in care homes are receiving antipsychotics, even when inappropriately prescribed. A third of people with dementia who go into hospital come out with reduced functional ability.
The statistics on poor quality care do indeed reflect the general picture reported in England from the Care Quality Commission.
OECD and WHO have been formulating a framework for dementia care across countries, providing a way of measuring good care and measuring progress. This framework describes building action on strengthening domestic systems of health and social care. This is particularly pertinent in England where social care has been progressively cut in the last few years. Secondly, Pearson outlined the need to develop good policies; thirdly to measure progress.
10 different stages were then presented.
They move from risk reduction to delivery of diagnosis, to early stages, to support in the communities, the possible transfer to an institution, and finally end of life and palliative care; cross cutting issues including the intelligent use of technology.
Pearson then described the rôle of people in dementia care; the need to focus on personal interactions, a key factor in determining the quality of life.
“We do need to support the people who do the support.” Counselling, training, respite need to be targeted for carers; including low prestige and poor employment conditions. I personally am hoping that Andy Burnham MP can forge ahead with this in beefing up training of the workforce, as well as producing some rights for caregivers in the NHS Constitution.
Pearson also outlined the need for care coordination, between health and social care systems. There need to be better data sharing, electronic patient records, better coordination, for example, Pearson argues; and I could not agree more. Progress will be made in England, I believe, through whole person care.
Pearson emphasised the need to measure the quality of care, as a benchmarking of performance across different providers, in different countries; to measure policies, activities, and outcomes, systematically, as Pearson argues, for people living with dementia and caregivers.
The new OECD report can be found here.
Rosa did a much needed introduction to the importance of human rights.
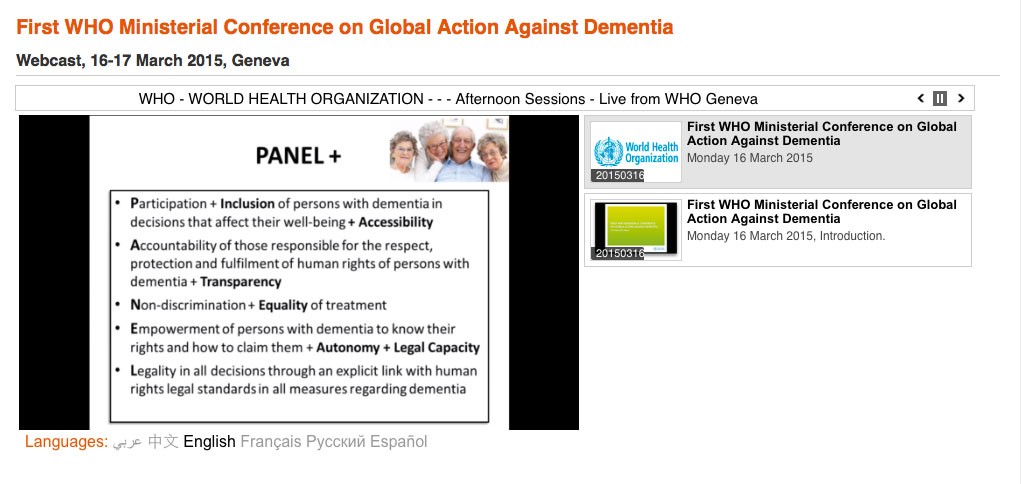
Rosa introduced ‘PANEL’ – for the need for all stakeholders to consider in policy (e.g. as for Scotland).
People with dementia should be able to enjoy their rights and freedoms, to ensure dignity and privacy.



Shibley, are “carers” those employed in community services and “caregivers” care partners/supporters like me? Or the other way round?
We badly need both a trained care workforce, and education n’ training for care partners and PWD peri- and post-diagnosis.