The picture above was taken at Ljubljana in Slovenia where we had the 25th Alzheimer Europe conference on the theme of “Dementia: Putting strategies and research into practice”.
Perhaps one of the most overused terms of the century is ‘breaking down the silo’. I don’t know enough about the engineering of silos to comment, thankfully.
I wish to explain in my blogpost here the overall direction of travel for my final book to do with dementia. Like the previous books, it will be heavily guided by the current literature from the brilliant people doing dementia research around the world. This research comes from a number of different angles as usual: looking for therapies for particular dementias, as well as research which is more geared towards economics, law, psychology, or cognitive neuroscience. And crucially the lived experiences – great, good, and bad.
My final book will be on enhancing health in dementia. Health is not simply the absence of illness and disease, and the books will resume the social model of disability not the biomedical model. For my book, I will need to draw on current evidence and guidelines particularly from the medicine and nursing professions nonetheless, but only as relevant to “the big picture”.
The topics will mark a clear departure from my previous books ‘Living well with dementia: the importance of the person and the environment’ and ‘Living better with dementia: good practice and innovation” in some areas. There can be no denying that persons living with dementia in residential homes and at home are also living as part of “dementia friendly communities”.
I am particularly mindful of imminent developments in quality of post diagnostic support from the Alzheimer’s Society, Dementia UK, Care England, Care Quality Commission and NHS England.
Book 1
Details here
Book 2
Details here
Prof Sube Banerjee, Professor for Dementia at Brighton and Sussex Medical School, has kindly agreed to write the main Foreword for my third book. Sube will be joined by Lisa Rodrigues, formerly chief executive of Sussex Foundation Partnership Trust. Joining both Sube and Lisa will be Lucy Frost, clinical nursing specialist and campaigner.
They in fact join a great line up of brilliant people who have contributed forewords to my previous two books: namely, Kate Swaffer, Chris Roberts, Beth Britton, Prof Facundo Manes, Prof John Hodges and Sally Marciano.
The first book was written around the NICE Quality Standard 30 on “Supporting people to live well with dementia”. It was written just after the hugely successful Prime Minister’s Dementia Challenge, which coincided with a strong leadership drive to do with dementia around the world including the G8 and G7 legacy events. Another major event was the one hosted by WHO and Alzheimer’s Disease International in Geneva in March 2015.
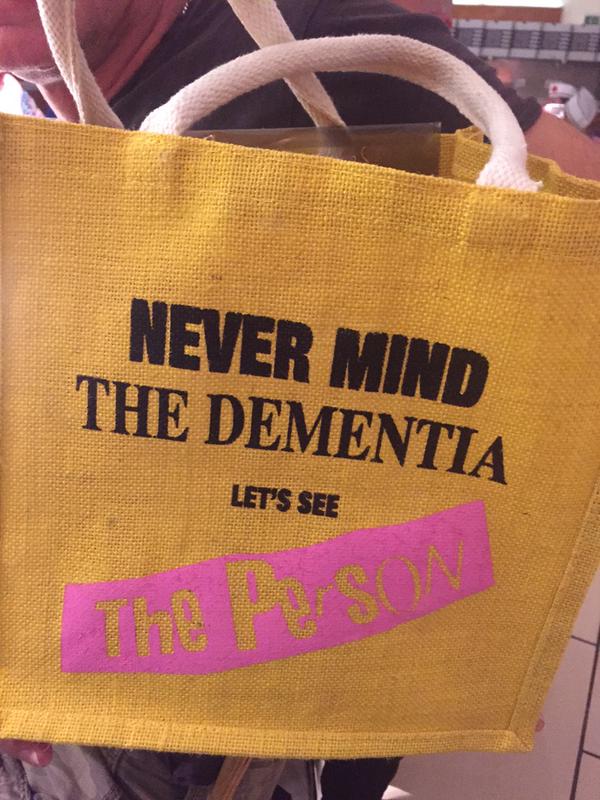
My first book had a bias towards English dementia policy. My second book took a much more holistic view, and indeed included two chapters on global dementia strategies and diversity. In my second book, I introduced the importance of integrated care and whole person care in ‘seeing the person, not the dementia’.
In my third book, I will need to come back to recent service innovations in England, including the ‘vanguards’ and the ‘new models of care’. There is however a tendency though to be attracted to the ‘new and exciting’, and not to give proper scrutiny to on-running threads in policy.
It is going to be necessary to refer both to the developments in England’s policy, including also developments in system redesigns offering better value and system leadership, in my third book. I would also like to draw on best practice from other countries, for example the Alzheimer Society of Ireland’s anti-stigma campaign, or Scotland’s ‘Focus on Dementia’. The lead given on person-centred dementia care by ALLIANCE Scotland will be reflected.
There are a number of workstreams in Europe which are particularly relevant to this third book. I wish to address fairly addressing the health needs of persons living with dementia, whether in care at home or in a residential setting (such as a care home or nursing home). I should like this book also to retain the strong human rights theme developed in book 2, with discussion of how the UN Convention on Rights for Persons with Disabilities could be applied for dementia around the world.
My hope for the third book, like the previous books, will be that the content will be quite generic. It is hoped that I will showcase some of the outstanding work that has recently begun to emerge in journals and at conferences. I myself have been to, and spoken at, a number of conferences in 2015. This has been enormously helpful for me in weighing up the ‘hot topics’ for my book.
Quality of care is the overriding theme of my book. In keeping with parity of esteem, I wish to address aspects of mental health in a wide context (e.g. insight, effects of sleep hygiene, anxiety and depression) on a par with physical health (e.g. infections, frailty, fall, fractures).
I introduced rehabilitation and recovery in book 2, and I wish to elaborate on this work in discussion of life story, reminiscence, cognitive stimulation therapy, and wider approaches.
I wish to look at the overused phrase ‘meaningful activities’, and to think about the place of these activities in both care at home and in residential homes.
I will look at the importance of relationships not only between residents and others to improve quality of life and care but also between staff to improve leadership and staff skills. I will also consider intimate relationships and sexuality, and spirituality.
All patients in all care settings in this jurisdiction are entitled to the best standards of NHS and social care, and certainly free from abuse and neglect. Intelligent use of technology is paramount for integrated care, including electronic health records and mitigation against prescribing errors. Many persons with dementia live with important co-morbidity, and technology is an important consideration in self-management.
For an integrated health and care system to work, persons with dementia should attend acute care only when necessary, care transitions should be facilitated as should patient flow and appropriate use of other healthcare settings. Careful case management including dementia advisors, dementia support workers and clinical nursing specialists, will be extremely important.
I intend to devote a chapter to end of life, particularly drawing on high quality research from palliative medicine. I wish to consider advance care planning, difficult conversations, anticipatory grief, reactions of residents, place of death, end of life in residential care, and dementia as a terminal disease.
Finally, it cannot be assumed that all persons living with dementia ultimately wish to live in a care home. Therefore, I will consider care at home, respite care, living alone with dementia; as well as possible future developments in extra care housing, smart homes, and the implications for the ‘aging in place’ policy strand.
I am hoping to cover this all in thirteen chapters in about 300 pages. I do not wish to promote any particular chain of care homes, but I would like to provide case studies of great practice. It is my intention to continue consulting as widely as possible. As regulation is a pervasive theme in this book, I intend to meet up with Andrea Sutcliffe from the Care Quality Commission. I also intend to liaise closely with people who have experienced the services in different regions of the UK including Wales, through, for example, voluntary sector organisations such as Age UK.