This study can only take place subject to ethical approval from a local COREC. Whilst there is no wish to collect data apart from anonymously, and whilst we will ensure governance of the study for data collection, information given to participants, and whilst we will seek permission to take part (and consent), it’s imperative that a senior investigator on the team (not me) is accountable for the findings. This will be essential if we are later to publish any findings publicly in abstract form or beyond.
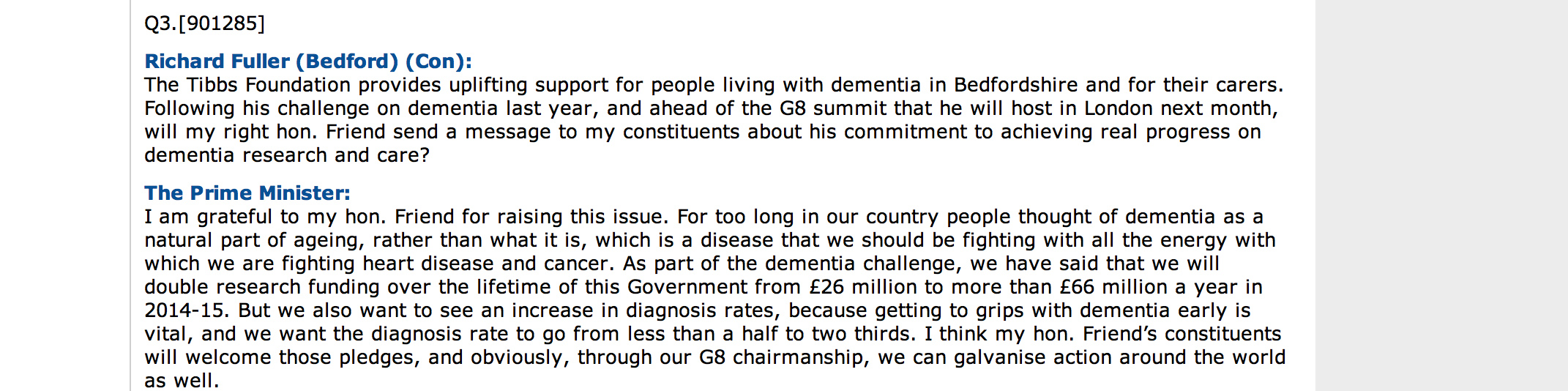
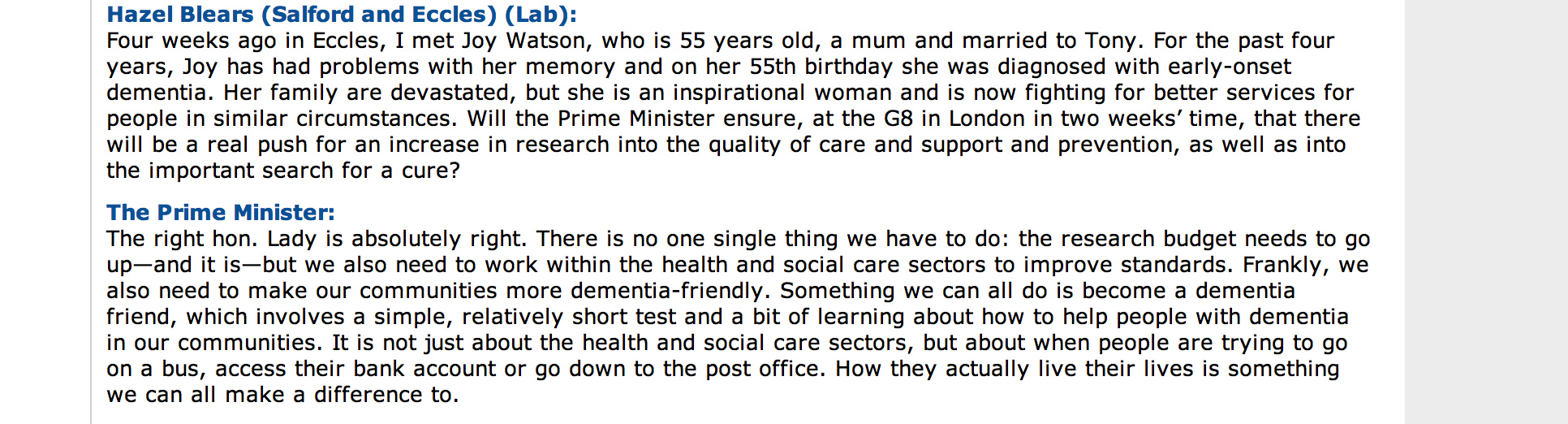
I am intrigued about personal reactions to the #G8dementia summit, regarding some perceptions and the image of dementia, and whether the summit addressed any of that.
I’m also interested in seeing whether the summit had a differential effect on those persons living with dementia, and those without (including carers).
There are 28 questions.
Some invite open-ended answers.
There’ll therefore be three groups:
Group A Persons living with dementia
Group B Carers
Group C Not groups A or B
I’ll make three links to these 3 surveys available in time.
I’d be interested in any changes to the questions, or any additions to this list of questions. I will be also collecting very basic demographic data in my surveys. Please use the comments section below this post.
THE SURVEY
This survey is about your perceptions and image of the G8 Dementia Summit which took place in December 2013.
This survey is completely anonymous.
I’d be very grateful if you could answer as best as you can.
The questions have no right/wrong answers.
The survey is in three sections: Part A, B and C.
Thanks!
PART A
Questions 1 – 19
1. Did you see any of the news coverage on the television about the #G8dementia Conference last year?
Yes
No
2. Did you hear any of the news coverage on the radio about the #G8dementia Conference last year?
Yes
No
3. Did you read any of the news coverage on the internet about the #G8dementia Conference last year? This could include any references to the event in the social media, such as Facebook or Twitter.
Yes
No
4. Were you aware of a potential significance of dementia in the future?
Yes
No
5. Do you consider the response against dementia to be a ‘fight’?
Yes
No
6. Do you consider the numbers of people to be living with dementia to be a ‘explosion’ in the near future?
Yes
No
7. Do you consider yourself to be ‘shocked’ by dementia?
Yes
No
8. a) Do you think it’s right to compare dementia to HIV/AIDS?
Yes
No
Not sure
b) Please provide further details, particularly if you were unable to produce a clear ‘yes’ or ‘no’ answer.
[open ended]
9. a) Do you think it’s right to compare dementia to cancer?
Yes
No
Not sure
b) Please provide further details, particularly if you were unable to produce a clear ‘yes’ or ‘no’ answer.
[open ended]
10. a) Do you consider the response against dementia to be a ‘war’?
Yes
No
Not sure
b) Please provide further details, particularly if you were unable to produce a clear ‘yes’ or ‘no’ answer.
[open ended]
11. a) Do you consider the response against dementia to be a ‘flood’, or something against which ‘the tide must be turned’?
Yes
No
Not sure
b) Please provide further details, particularly if you were unable to produce a clear ‘yes’ or ‘no’ answer.
[open ended]
12. Did the #G8dementia summit evoke in you a feeling of being ‘fearful’ about dementia?
Yes
No
13. Did the #G8dementia summit evoke in you a feeling of being ‘excited’ about social care for dementia?
Yes
No
14. Did the #G8dementia summit evoke in you a feeling of being ‘excited’ about the possibility of a breakthrough in a cure for dementia?
Yes
No
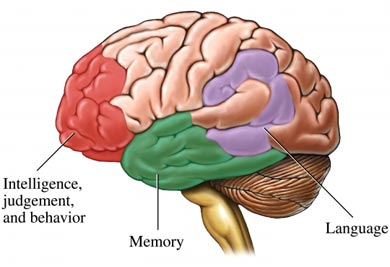
15. Did the #G8dementia leave you clearer about the relationship between Alzheimer’s disease and dementia?
Yes
No
16. a) The #G8dementia sought to improve research and a lot of this focussed on ‘personalised medicine’. Did you feel this was explained to you so that you understand it better following the G8?”
Yes
No
b) Please elaborate if you wish.
[open ended]
17. The research community is absolutely clear about the distinction between normal ageing and disease: agree or disagree?
Yes
No
18. Do you feel that #G8dementia addressed the notion that people do not always have the right knowledge and information to manage their condition?
Yes
No
19. Do you feel that #G8dementia promoted ‘living well with dementia’, for example through health innovations?
Yes
No
PART B
Question 20
20. How well do you think the #G8dementia Conference did in addressing the needs of the following groups of the following people?
[Answer from 0 (not at all) to 5 (completely)]
Researchers
Pharma Industry
Persons with dementia
Carers of persons with dementia
Journalists and the media
Politicians
Big charities
Small charities
PART C
Questions 21 – 28
21. What do you believe the #G8dementia summit set out to achieve? Did the organisers achieve in their aims?
[open ended]
22. Do you have any concerns about the way the #G8dementia summit was conducted?
[open ended]
23. What do you expect the #G8dementia summit, in fact, will achieve ultimately?
[open ended]
24. Do you think the #G8dementia helped decrease the stigma which has been associated with dementia?
[open ended]
25. Do you feel the public is generally united in their perceptions of dementia, or do you there exists a diverse range of different perceptions?
[open ended]
26. Do you think negative perceptions of perception exist by members of the public? Why or why not?
[open ended]
27. Are there any positive perceptions of perception by members of the public?
[open ended]
28. Finally, do you have any views about what the aim or purpose of the #G8dementia summit was? Do you know how it was instigated, and by whom?
[open ended]