These are the references to Chapter 1 “Introduction”, mainly an overview of English dementia policy, prevention and risk factors, for my new book, “Living better with dementia: championing change for the future” (to be published early 2014).
Websites
“Call to action: the use of antipsychotics for people with dementia” http://www.institute.nhs.uk/qipp/calls_to_action/Dementia_and_antipsychotic_drugs.html
A letter to the Prime Minister charting progress on the Prime Minister’s Dementia Challenge (dated 7th May 2014). https://s3-eu-west-1.amazonaws.com/media.dh.gov.uk/network/353/files/2014/05/10092-2902335-TSO-Dementia-Letter-to-PM-ACCESSIBLE.pdf
All Party Parliamentary Group (APPG) on dementia. (2012) Unlocking the diagnosis: the key to improving the lives of people with dementia http://www.alzheimers.org.uk/site/scripts/download_info.php?fileID=1457 (dated June)
Dementia 2013: The hidden voice of lonelineness http://www.alzheimers.org.uk/dementia2013
Dementia Roadmap. http://dementiaroadmap.info
Department of Health (2012) Prime Minister’s Dementia Challenge: delivering major improvements in dementia care and research by 2015 https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/215101/dh_133176.pdf
Making a Difference in Dementia: Nursing Vision and Strategy https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/147956/Making_a_Difference_in_Dementia_Nursing_Vision_and_Strategy.pdf
Memory Services National Accreditation Programme (Royal College of Psychiatrists) http://www.rcpsych.ac.uk/workinpsychiatry/qualityimprovement/qualityandaccreditation/memoryservices/memoryservicesaccreditation.aspx
NHS Confederation website/NHS Voices blog. (2014) A people-centred response to the 2015 Challenge is vital for the future of health and care, says Jeremy Taylor, http://www.nhsconfed.org/blog/2014/06/a-people-centred-response-to-the-2015-challenge-is-vital-for-the-future-of-health-and-care
PM Challenge on dementia (Alzheimer’s Research UK) http://www.alzheimersresearchuk.org/news-detail/10688/PM-Challenge-on-Dementia-a-year-of-progress-and-new-promise-for-research/ (dated 15 May 2013)
Public Health England and UK Health Prevention First (2014). The Blackfriars Consensus on promoting brain health: reducing risks for dementia in the population http://nhfshare.heartforum.org.uk/RMAssets/Reports/Blackfriars%20consensus%20%20_V18.pdf (“Blackfriars Consensus Statement”)
Rahman, S. (2014) “It’s time we talked about ‘dementia friendly communities’” Living well with dementia blog, http://livingwelldementia.org/2014/03/25/its-time-we-talked-about-dementia-friendly-communities/ (25th March 2014).
Report on the prescribing of anti-psychotic drugs to people with dementia (author: Professor Banerjee) http://webarchive.nationalarchives.gov.uk/20130107105354/http:/www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_108303 (November 2009)
WHO (2013) [ed. Wilkinson, R., Marmot, M.] Social determinants of health: the solid facts. http://www.euro.who.int/__data/assets/pdf_file/0005/98438/e81384.pdf
Other references
Ahlskog, J.E., Geda, Y.E., Graff-Radford, N.R., Petersen, R.C. (2011) Physical exercise as a preventive or disease-modifying treatment of dementia and brain aging, Mayo Clin Proc, 86(9), pp. 876–84.
Albert, M.S., DeKosky, S.T., Dickson, D., Dubois, B., Feldman, H.H., Fox, N.C,., Gamst, A., Holtzman, D.M., Jagust, W.J., Petersen, R.C., Snyder, P.J., Carrillo, M.C., Thies, B., Phelps, C.H. (2011) The diagnosis of mild cognitive impairment due toAlzheimer’s disease: recommendations from the National Institute on Aging–Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease, Alzheimers Dement, 7, pp. 270–9.
Alzheimer’s Association Expert Advisory Workgroup on NAPA (2012) Workgroup on NAPA’s scientific agenda for a national initiative on Alzheimer’s disease, Alzheimer Dement, 8, pp. 357–361.
Bambra, C., Gibson, M., Sowden, A., Wright, K., Whitehead, M., Petticrew, M. (2010) Tackling the wider social determinants of health and health inequalities: evidence from systematic reviews, J Epidemiol Community Health, Apr, 64(4), pp. 284-91.
Barberger-Gateau, P., Raffaitin, C., Letenneur, L., Berr, C., Tzourio, C., Dartigues, J.F., Alpérovitch, A. (2007) Dietary patterns and risk of dementia: the Three-City cohort study. Neurology, Nov 13, 69(20), pp. 1921-30.
Bennett, D.A., Schneider, J.A., Tang, Y., Arnold, S.E., Wilson, R.S. (2006) The effect of social networks on the relation between Alzheimer’s disease pathology and level of cognitive function in old people: a longitudinal cohort study, Lancet Neurol, 5(5), pp. 406–12.
Beydoun, M.A., Beydoun, H.A., Wang, Y. (2008) Obesity and central obesity as risk factors for incident dementia and its subtypes: a systematic review and meta-analysis, Obes Rev, 9, pp. 204–218.
Biessels GJ. Capitalising on modifiable risk factors for Alzheimer’s disease. Lancet Neurol, Aug, 13(8), pp. 752-3.
Black, S.E., Patterson, C. Feightner, J. (2001) Preventing dementia, Canadian Journal of Neurology Science, 28 (Suppl 1), pp. S56–66.
Blackburn, D.J., Krishnan, K., Fox, L., Ballard, C., Burns, A., Ford, G.A., Mant, J., Passmore, P., Pocock, S., Reckless, J., Sprigg, N., Stewart, R., Wardlaw, J., Bath, P.M. (2013) Prevention of Decline in Cognition after Stroke Trial (PODCAST): a study protocol for a factorial randomised controlled trial of intensive versus guideline lowering of blood pressure and lipids, Trials, Nov 22, 14: 401.
Bond, J. (1992) The medicalization of dementia, Journal of Aging Studies, 6, 397–403.
Bowling, A. (2007) Aspirations for old age in the 21st century, what is successful aging? The International Journal of Aging and Human Development, 64, 263–297.
Boyle, P.A., Buchman, A.S., Wilson, R.S., Yu, L., Schneider, J.A., Bennett, D.A. (2012) Effect of purpose in life on the relation between Alzheimer disease pathologic changes on cognitive function in advanced age, Arch Gen Psychiatry, 69(5), pp. 499– 505.
Brodaty, H., Howarth, G., Mant, A., Kurle, S. (1994) General practice and dementia, A national survey of Australian GPs, Medical Journal of Australia, 160, 10–14.
Brooker, D., La Fontaine, J., Bray, J., Evans, S. (for the University of Worcester Association of Dementia Studies) (2013), Timely diagnosis of dementia: ALCOVE WP5 Task 1 and 2.
Brunet M. (2014) Targets for dementia diagnoses will lead to over-diagnosis, BMJ, 348:g2224.
Brunnström, H., Gustafson, L., Passant, U., Englund, E. (2009) Prevalence of dementia subtypes: a 30-year retrospective survey of neuropathological reports, Arch Gerontol Geriatr, Jul Aug, 49(1), pp. 146-9.
Buchman, A.S., Wilson, R.S., Bienias, J.L., Shah, R.C., Evans, D.A., Bennett, D.A. (2005) Change in body mass index and risk of incident Alzheimer disease, Neurology, 65, pp. 892–897.
Burns, A., Robert, P. (2009) The National Dementia strategy in England, BMJ, Mar 10, 338:b931.
Chang, M., Jonsson, P.V., Snaedal, J., Bjornsson, S., Saczynski, J.S., Aspelund, T., Eiriksdottir, G., Jonsdottir, M.K., Lopez, O.L., Harris, T.B., Gudnason, V., Launer, L.J. (2010) The effect of midlife physical activity on cognitive function among older adults: AGES—Reykjavik study, J Gerontol A Biol Sci Med Sci, 65(12), pp. 1369–74.
Cooper, C. (2013) G8 Dementia Summit: PM pledges to double funding for research by 2025, 11 December 2013, The Independent newspaper, http://www.independent.co.uk/life-style/health-and-families/health-news/g8-dementia-summit-pm-pledges-to-double-funding-for-research-by-2025-8996377.html
Crampton, J., Dean, J., Eley, R. (2012) Joseph Rowntree Foundation: Creating a dementia friendly York, http://www.jrf.org.uk/sites/files/jrf/dementia-communities-york-full.pdf.
Cunningham, E.L., Passmore, A.P. (2013) Drug development in dementia, Maturitas, 76(3), pp. 260-6.
Daviglus, M.L., Bell, C.C., Berrettini, W., Bowen, P.E., Connolly, E.S. Jr, Cox, N.J., Dunbar-Jacob, J.M., Granieri, E.C., Hunt, G., McGarry, K., Patel, D., Potosky, A.L., Sanders-Bush, E., Silberberg, D., Trevisan, M. (2010) National institutes of health state-of-the-science conference statement: preventing Alzheimer disease and cognitive decline, Annals of Internal Medicine, August 3, 153(3), pp. 176–81.
De Lepeliere, J., Wind, A., Iliffe, S., Moniz-Cook, E., Wilcock, J., Gonzalez, V., Derksen, E., Gianelli, M., Vernooij-Dassen, M. the Interdem Group. (2008). The primary care diagnosis of dementia in Europe: An analysis using multi-disciplinary, multi-national expert groups, Aging & Mental Health, 12(5), 568–576.
Desmond, D.W., Tatemichi, T.K., Paik, M., Stern, Y. (1993) Risk factors for cerebrovascular disease as correlates of cognitive function in a stroke free cohort, Archives of Neurology, 50, pp. 162–166.
Devi, G., Ottman, R., Tang, M., Marder, K., Stern, Y., Tycko, B., Mayeux, R. (1999) Influence of APOE genotype on familial aggregation of AD in an urban population, Neurology, 53: 789.
Devore, E.E., Grodstein, F., van Rooij, F.J., Hofman, A., Stampfer, M.J., Witteman, J.C., Breteler M.M. (2010) Dietary antioxidants and long-term risk of dementia, Arch Neurol, Jul, 67(7), pp. 819-25.
Downs, M., Turner, S., Iliffe, S., Bryans, M., Wilcock, J., Keady, J. (2003) Improving the response of primary care practitioners to people with dementia and their families: A randomised controlled trial of educational interventions. Final Report to the UK Alzheimer’s Society, Bradford: UK Alzheimer’s Society.
EClipSE Collaborative Members, Brayne, C., Ince, P.G., Keage, H.A., McKeith, I.G., Matthews, F.E., Polvikoski, T., Sulkava, R. (2010) Education, the brain and dementia: neuroprotection or compensation? Brain, Aug, 133(Pt 8), pp. 2210-6.
Gao, S., Hendrie, H. C., Hall, K. S, Hui, S. (1998) The relationships between age, sex, and the incidence of dementia and Alzheimer disease: a meta-analysis, Archives of General Psychiatry, 55, 809–815.
Gauthier, S., Leuzy, A., Racine, E., Rosa-Neto, P. (2013) Diagnosis and management of Alzheimer’s disease: past, present and future ethical issues, Prog Neurobiol, Nov. 110:102-13.
Gustafson, D.R., Backman, K., Waern, M., Ostling, S., Guo, X., Zandi, P., Mielke, M.M., Bengtsson, C., Skoog, I. (2009) Adiposity indicators and dementia over 32 years in Sweden. Neurology, 73, pp. 1559–1566.
Haase, H., Rink, L. (2009) Functional significance of zinc-related signaling pathways in immune cells, Annu Rev Nutr, 29, pp. 133–152.
Håkansson, K., Rovio, S., Helkala, E.L., Vilska, A.R., Winblad, B., Soininen, H., Nissinen, A., Mohammed, A.H., Kivipelto, M., .Soininen H., Nissinen, A., Mohammed, A.H., Kivipelto, M. Association between mid-life marital status and cognitive function in later life: population based cohort study, BMJ, 339:b2462.
Hansen, E.C., Hughes, C., Routley, G., Robinson, A.L. (2008) General practitioners’ experiences and understandings of diagnosing dementia: factors impacting on early diagnosis, Soc Sci Med, Dec, 67(11), pp. 1776-83.
Harvey, R.J., Rossor, M.N., Skelton-Robinson, M. (1998) Young onset dementia: epidemiology, clinical symptoms, family burden, support and outcome, London: Dementia Research Group.
Hofman, A., Ott, A., Breteler, M.M., Bots, M.L., Slooter, A.J., van Harskamp, F, van Duijn, C.N., Van Broeckhoven, C., Grobbee, D.E. (1997) Atherosclerosis, apolipoprotein E, and prevalence of dementia and Alzheimer’s disease in the Rotterdam Study, Lancet, 349, pp. 151–154
Holland, W. (2012) Competition or collaboration? A comparison of health services in the UK, Clinical Medicine, 10(5), pp. 431–3
Imtiaz, B., Tolppanen, A.M., Kivipelto, M., Soininen. H. (2014) Future directions in Alzheimer’s disease from risk factors to prevention, Biochem Pharmacol, Apr 15, 88(4), pp. 661-70.
Innes, A., Manthorpe, J. (2013) Developing theoretical understandings of dementia and their application to dementia care policy in the UK, Dementia (London), Nov, 12(6), pp. 682-96.
Ionicioiu, I., David, D., Szamosközi, S. (2014) A quantitative meta-analysis of the effectiveness of psychosocial interventions in dementia, Procedia – Social and Behavioral Sciences, 27, pp. 591 – 594.
Jenkins, C.R., Thien, F.C.K., Wheatley, J.R., Reddel, H.K. (2005) Traditional and patient-centred outcomes with three classes of asthma medication, European Respiratory Journal, 26(1), pp. 36-44.
Jiang, T., Yu, J.T., Tian, Y., Tan, L. (2013) Epidemiology and etiology of Alzheimer’s disease: from genetic to non-genetic factors, Curr Alzheimer Res, Oct, 10(8), pp. 852-67.
Johansson, L., Guo, X., Waern, M., Ostling, S., Gustafson, D., Bengtsson, C., Skoog, I. (2010) Midlife psychological stress and risk of dementia: a 35-year longitudinal population study. Brain, Aug, 133(Pt 8), pp. 2217-24.
Jorm, A.F., Jolley, D. (1998) The incidence of dementia: a meta-analysis, Neurology, 51, 728–33.
Kehne, J.H. (2007) The CRF1 receptor, a novel target for the treatment of depression, anxiety, and stress-related disorders, CNS Neurol Disord Drug Targets, 6, pp. 163–182.
Khachaturian, A.S., Meranus, D.H., Kukull, W.A., Khachaturian, Z.S. (2013) Big data, aging, and dementia: pathways for international harmonization on data sharing, Alzheimers Dement, 9 (5 Suppl), pp. S61-2.
Khachaturian, Z.S., Petersen, R.C., Snyder, P.J., Khachaturian, A.S., Aisen, P., de Leon, M., Greenberg, B.D., Kukull, W., Maruff, P., Sperling, R.A., Stern, Y., Touchon, J., Vellas, B., Andrieu, S., Weiner, M.W., Carrillo, M.C., Bain, LJ. (2011) Developing a global strategy to prevent Alzheimer’s disease: Leon Thal Symposium 2010, Alzheimers Dement, Mar, 7(2), pp. 127-32.
Kim, J.W., Lee, D.Y., Lee, B.C., Jung, M.H., Kim, H., Choi, Y.S., Choi, I.G. (2012) Alcohol and cognition in the elderly: a review, Psychiatry Investig, Mar, 9(1), pp. 8-16.
Kivipelto, M., Ngandu, T., Fratiglioni, L., Viitanen, M., Kareholt, I., Winblad, B., Helkala, E.L., Tuomilehto, J., Soininen, H., Nissinen, A. (2006) Obesity and vascular risk factors at midlife and the risk of dementia and Alzheimer disease, Arch Neurol, 62, pp. 1556–1560.
Kmietowicz, Z. (2012) Cameron launches challenge to end “national crisis” of poor dementia care, BMJ, 344, e2347.
Kmietowicz, Z. (2014) Recorded diagnosis of dementia in England increases by 62% since 2006, BMJ, 349, g4911.
Koch, T., Iliffe, S. (2011) Implementing the National Dementia Strategy in England: Evaluating innovative practices using a case study methodology, Dementia, 10(4) 487–498.
Kopelman, P.G., (2000) Obesity as a medical problem, Nature, 404, pp. 635–643.
Lautenschlager, N.T., Cupples, L.A., Rao, V.S., Auerbach, S.A., Becker, R., Burke, J., Chui, H., Duara, R., Foley, E.J., Glatt, S.L., Green, R.C., Jones, R., Karlinsky, H., Kukull, W.A., Kurz, A., Larson, E.B., Martelli, K., Sadovnick, A.D., Volicer, L., Waring, S.C., Growdon, J.H., Farrer, L.A. (1996) Risk of dementia among relatives of Alzheimer’s disease patients in the MIRAGE study: What is in store for the oldest old? Neurology, 46, pp. 641–50.
Leonard BE. (2006) HPA and immune axes in stress: involvement of the serotonergic system. Neuroimmunomodulation, 13, pp. 268–76.
Lieb, W., Beiser, A.S., Vasan, R.S., Tan, Z.S., Au, R., Harris, T.B., Roubenoff, R., Auerbach, S., De- Carli, C., Wolf, P.A., Seshadri, S. (2009) Association of plasma leptin levels with incident Alzheimer disease and MRI measures of brain aging, JAMA, 302, pp. 2565–2572.
Ligthart, S.A., Moll van Charante, E.P., van Gool, W.A., Richard, E. (2010) Treatment of cardio-vascular risk factors to prevent cognitive decline and dementia: a systematic revie, Vascular Health & Risk Management, (6), pp. 775–85.
Lincoln, P., Fenton, K., Alessi, C., Prince, M., Brayne, C., Wortmann, M., Patel, K., Deanfield, J., Mwatsama, M. (2014) The Blackfriars Consensus on brain health and dementia, Lancet, May 24, 383(9931), pp. 1805-6.
Lindsay, J., Hebert, R.Rockwood, K. (1997) The Canadian Study of Health and Aging – Risk Factors for Vascular Dementia, Stroke, 28, 526–530.
Lupton, D. (1999) Risk. London: Routledge.
Lyman, K. A. (1989) Bringing the social back in: a critique of the bio-medicalisation of dementia, Gerontologist, 29, pp. 597–604.
Masi, C.M., Chen, H.Y., Hawkley, L.C., Cacioppo, J.T. (2011) A meta-analysis of interventions to reduce loneliness, Pers Soc Psychol Rev, Aug, pp. 15(3):219-66.
McCullagh, C.D., Craig, D., Mollroy, S.P., Passmore, A.P. (2001) Risk factors for dementia, Advances in Psychiatric Treatment, 7, pp. 24-31.
McKhann, G.M, Knopman, D.S., Chertkow, H., Hyman, B.T., Jack, C.R. Jr, Kawas, C.H., Klunk, W.E., Koroshetz, W.J., Manly, J.J., Mayeux, R., Mohs, R.C., Morris, J.C., Rossor, M.N., Scheltens, P., Carrillo, M.C., Thies, B., Weintraub, S., Phelps, C.H. (2011) The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging–Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease, Alzheimers Dement, 7, pp. 263–9.
Milne, A. (2010) Dementia screening and early diagnosis: The case for and against, Health, Risk & Society, 12(1), pp. 65–76.
Mizutani, K., Nishimura, K., Ichihara, A., Ishigooka, J. (2014) Dissociative disorder due to Graves’ hyperthyroidism: a case report, Gen Hosp Psychiatry, Mar 19. pii: S0163 8343(14)00073-5.
Monastero, R., Mangialasche, F., Camarda, C., Ercolani, S., Camarda, R. (2009) A systematic review of neuropsychiatric symptoms in mild cognitive impairment, J Alzheimers Dis, 18(1), pp. 11–30.
Moroney, J.T., Tang, M.X., Berglund, L., Small, S., Merchant, C., Bell, K., Stern, Y., Mayeux, R. (1999) Low density lipoprotein cholesterol and the risk of dementia with stroke, Journal of the American Medical Association, 282, pp. 254–260.
Morris, J.C. (2005) Early-stage and preclinical Alzheimer disease, Alzheimer Dis Assoc Disord, 19, pp. 163–5.
Morris, M.C., Evans, D.A., Bienias, J.L., Tangney, C.C., Bennett, D.A, Aggarwal, N., Schneider, J., Wilson, R.S. (2003) Dietary fats and the risk of incident Alzheimer disease, Arch Neurol, 60(2), pp. 194-200. [Erratum in: Arch Neurol. 2003 Aug;60(8):1072.]
National Audit Office (2007) Improving services and support for people with dementia, London: The Stationary Office.
Ngandu, T., Helkala, E.L., Soininen, H., Winblad, B., Tuomilehto, J., Nissinen, A., Kivipelto, M. (2007) Alcohol drinking and cognitive functions: findings from the Cardiovascular Risk Factors Aging and Dementia (CAIDE) Study, Dement Geriatr Cogn Disord, 23(3), pp. 140-9.
Ngandu, T., von Strauss, E., Helkala, E.L., Winblad, B., Nissinen, A., Tuomilehto, J., Soininen, H., Kivipelto, M. (2007) Education and dementia: what lies behind the association? Neurology, Oct 2, 69(14), pp. 1442-50.
Norton, S., Matthews, F.E., Barnes, D.E., Yaffe, K., Brayne, C. (2014) Potential for primary prevention of Alzheimer’s disease: an analysis of population-based data, Lancet Neurol, Aug, 13(8), pp. 788-94.
Panza, F., Frisardi, V., Seripa, D., Logroscino, G., Santamato, A., Imbimbo, B.P., Scafato, E., Pilotto, A., Solfrizzi, V. (2012) Alcohol consumption in mild cognitive impairment and dementia: harmful or neuroprotective? Int J Geriatr Psychiatry, Dec, 27(12):1218-38.
Peters, R. (2012) Blood pressure, smoking and alcohol use, association with vascular dementia. Exp Gerontol, Nov, 47(11), pp. 865-72.
Piazza-Gardner, A.K., Gaffud, T.J., Barry, A.E. (2013) The impact of alcohol on Alzheimer’s disease: a systematic review, Aging Ment Health, 17(2), pp. 133–46.
Prasad, A.S. (2009) Impact of the discovery of human zinc deficiency on health, J Am Coll Nutr, 28, pp. 257–265.
Prasad, A.S. (2003) Zinc deficiency, BMJ, 326, pp. 409–410.
Ratnavalli E, Brayne C, Dawson K, et al. (2002) The prevalence of frontotemporal dementia. Neurology, 58:1615–21.
Redman, R.W., Lynn, M.R. (2004) Advancing patient-centred care through knowledge development, Canadian Journal of Nursing Research, 36(3), pp. 116-129.
Rissman, R.A., Staup, M.A., Lee, A.R., Justice, N.J., Rice, K.C., Vale, W., Sawchenko, P.E. Corticotropin releasing factor receptor-dependent effects of repeated stress on tau phosphorylation, solubility, and aggregation, Proc Natl Acad Sci USA, Apr 17, pp. 109(16):6277-82.
Ritchie, C.W., Ritchie, K. (2012) The PREVENT study: a prospective cohort study to identify mid-life biomarkers of late-onset Alzheimer’s disease, BMJ Open, Nov 19, pp. 2(6).
Rusanen, M., Rovio, S., Ngandu, T., Nissinen, A., Tuomilehto, J., Soininen, H., Kivipelto, M. (2010) Midlife smoking, apolipoprotein E and risk of dementia and Alzheimer’s disease: a population-based cardiovascular risk factors, aging and dementia study. Dement Geriatr Cogn Disord, 30(3), pp. 277-84.
Saleem, A., Sophia, R. (2014) Voltage-gated potassium channel antibody-associated limbic encephalitis, Age Ageing, Jul, 43(4), pp. 583-5.
Sapolsky, R.M. (1996) Why stress is bad for your brain, Science, 273, pp. 749–50.
Scarmeas, N., Stern, Y., Tang, M.X., Mayeux, R., Luchsinger, J.A. (2006) Mediterranean diet and risk for Alzheimer’s disease, Ann Neurol, Jun, 59(6), pp. 912-21.
Schliebs, R., Arendt, T. (2011) The cholinergic system in aging and neuronal degeneration, Behav Brain Res, Aug 10, 221(2), pp. 555-63.
Skoog, I., Kalaria, R.N., Breteler, M.M. (1999) Vascular factors and Alzheimer disease, Alzheimer Dis Assoc Disord, 13(suppl 3), pp. S106–S114
ofi, F., Valecchi, D., Bacci D., Abbate, R., Gensini, G.F., Casini, A., Macchi, C. (2011) Physical activity and risk of cognitive decline: a meta-analysis of prospective studies, J Intern Med, 269(1), pp. 107–17.
Sperling, R.A., Rentz, D.M., Johnson, K.A., Karlawish, J., Donohue, M., Salmon, D.P., Aisen, P. (2014) The A4 study: stopping AD before symptoms begin? Sci Transl Med, Mar 19, 6(228), pp. 228fs13.
Stern, Y., Gurland, B., Tatemichi, T.K., Tang, M.X., Wilder, D., Mayeux, R. (1994) Influence of education and occupation on the incidence of Alzheimer’s disease, JAMA, 271(13), pp. 1004–10.
Szewczyk, B. (2013) Zinc homeostasis and neurodegenerative disorders. Front Aging Neurosci, Jul 19, 5:33.
Tischler V, D’Silva K, Cheetham A, Goring M, Calton T. Involving patients in research: the challenge of patient-centredness, Int J Soc Psychiatry, 2010 Nov, 56(6), pp. 623-33
Tyas, S.L., White, L.R., Petrovitch, H., Webster Ross, G., Foley, D.J., Heimovitz, H.K., Launer, L.J. (2003) Mid-life smoking and late-life dementia: the Honolulu-Asia aging study, Neurobiol Aging, 24(4), pp. 589–96.
van der Linde, R.M., Stephan, B.C., Matthews, F.E., Brayne, C., Savva, G.M. (2013) Medical Research Council Cognitive Function and Ageing Study. The presence of behavioural and psychological symptoms and progression to dementia in the cognitively impaired older population, Int J Geriatr Psychiatry, Jul;28(7):700-9.
van Duijn, C.M., Hendriks, L., Cruts, M., Hardy, J.A., Hofman, A. (1991) Amyloid precursor protein gene mutation in early-onset Alzheimer’s disease, Lancet, 337(8747): 978.
Vellas, B., Gillette-Guyonnet, S., Andrieu, S. (2008) Memory health clinics-a first step to prevention, Alzheimers Dement, Jan, 4(1 Suppl 1):S144-9.
van El, C.G., Cornel, M.C., Borry, P., Hastings, R.J., Fellmann, F., Hodgson, S.V., Howard, H.C., Cambon-Thomsen, A., Knoppers, B.M., Meijers-Heijboer, H., Scheffer, H., Tranebjaerg, L., Dondorp, W., de Wert, GM, ESHG Public and Professional Policy Committee. (2013) Whole-genome sequencing in health care: recommendations of the European Society of Human Genetics, Eur J Hum Genet, Jun;21(6):580-4.
Verity, C.M., Nicoll, A., Will, R.G., Devereux, G., Stellitano, L. (2000) Variant Creutzfeldt-Jakob disease in UK children: a national surveillance study, Lancet, Oct 7, 356(9237), pp. 1224-7.
Victor, M., Adams, R.D., Collins, G.H. (1971) The Wernicke–Korsakoff syndrome. F.A. Davis.
Vileland, T. (2002) Managing chronic disease: evidence-based medicine or patient-centred medicine? Health Care Analysis, 10(3), pp. 289-98.
Wang, H.X., Gustafson, D.R., Kivipelto, M., Pedersen, N.L., Skoog, I., Windblad, B., Fratiglioni, L. (2012) Education halves the risk of dementia due to apolipoprotein ε4 allele: a collaborative study from the Swedish brain power initiative, Neurobiol Aging, 33(5). 1007.e1-7.
Warren, M.W., Hynan, L.S., Weiner, M.F. (2012) Lipids and adipokines as risk factors for Alzheimer’s disease, J Alzheimers Dis, 29, pp. 151–157.
WHO (Revised February 2012) Variant Creutzfeldt-Jakob disease: factsheet no 180, available at http://www.who.int/mediacentre/factsheets/fs180/en/ [accessed 12 June 2014].
Wilson, R.S., Scherr, P.A., Schneider, J.A., Tang, Y., Bennett, D.A. (2007) Relation of cognitive activity to risk of developing Alzheimer disease, Neurology, 69(20), pp. 1911–20.
Wise J. (2014) £90m package to improve dementia care is announced in England, BMJ, 348, g1879.
Zecca, L., Youdim, M.B., Riederer, P., Connor, J.R., Crichton, R.R. (2004) Iron, brain ageing and neurodegenerative disorders, Nat Rev Neurosci, 5, pp. 863–873.
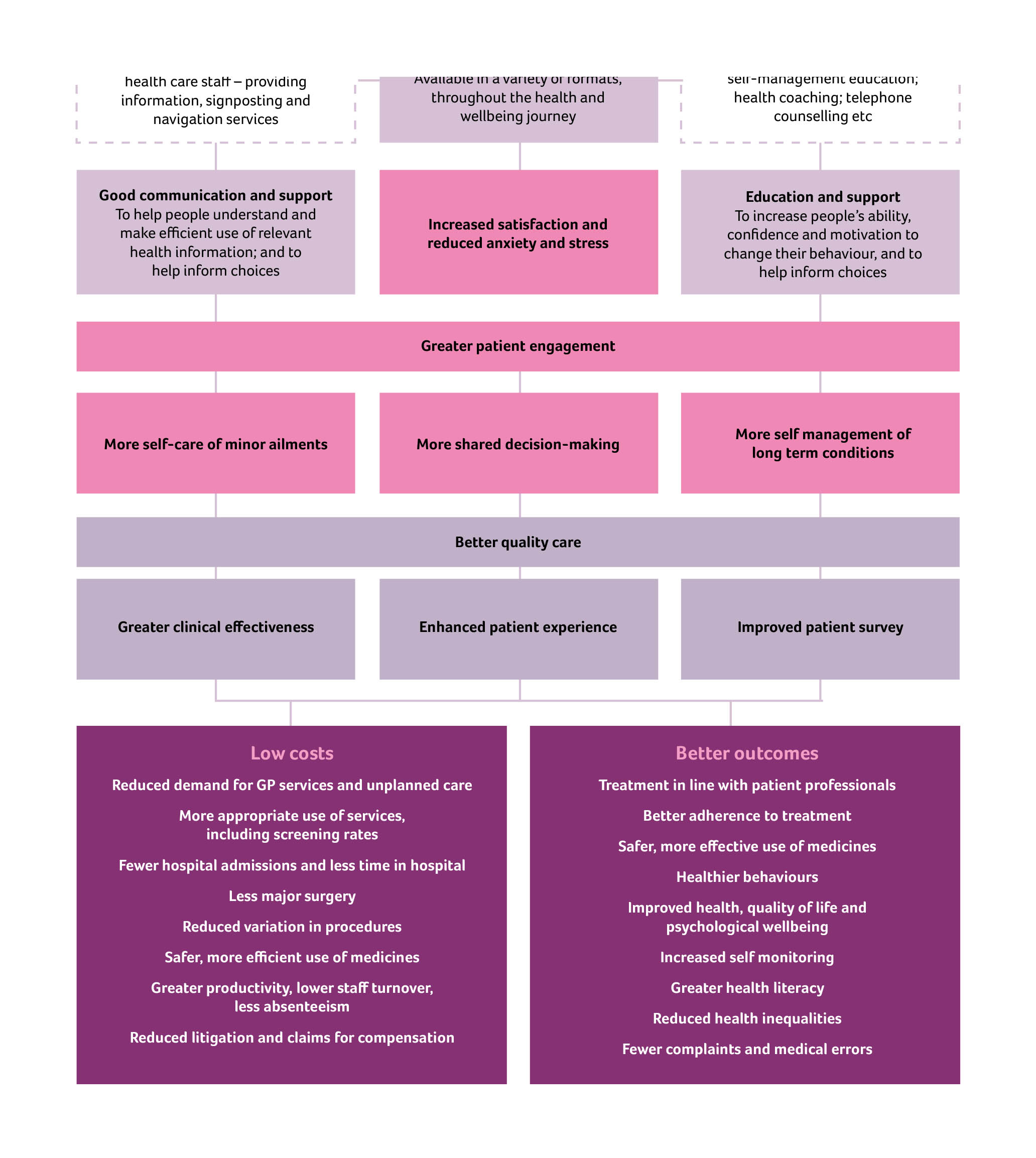
Source of the graphic in the top left corner of this page is here.