There was a time when the GP used to be at the heart of a person’s community, as well as ‘delivering care’. For some people, there is no such thing as society, and the community consists of high street brands, banks and services (such as police or fire).
I’ve spent some time thinking about the implementation of the ‘dementia friendly community’ policy in a number of jurisdictions. It really has struck me how, for whatever political reasons, nurses are not perceived to be the heart of dementia friendly communities in England.
This, I feel, is a great tragedy. I don’t deny there are about a hundred different causes of a dementia, people’s social circumstances will differ (it is not uncommon for a female widower to develop a dementia while very lonely), cultural differences exist (for example in the rôle of the family in those of an Asian background), there are different rates of progression, and so on.
On receiving a diagnosis, I think support services in dementia should be much stronger than now. What is all too commonplace is a travesty. People don’t know where to turn to for basic information about clinical aspects, or wider aspects about living in the community.
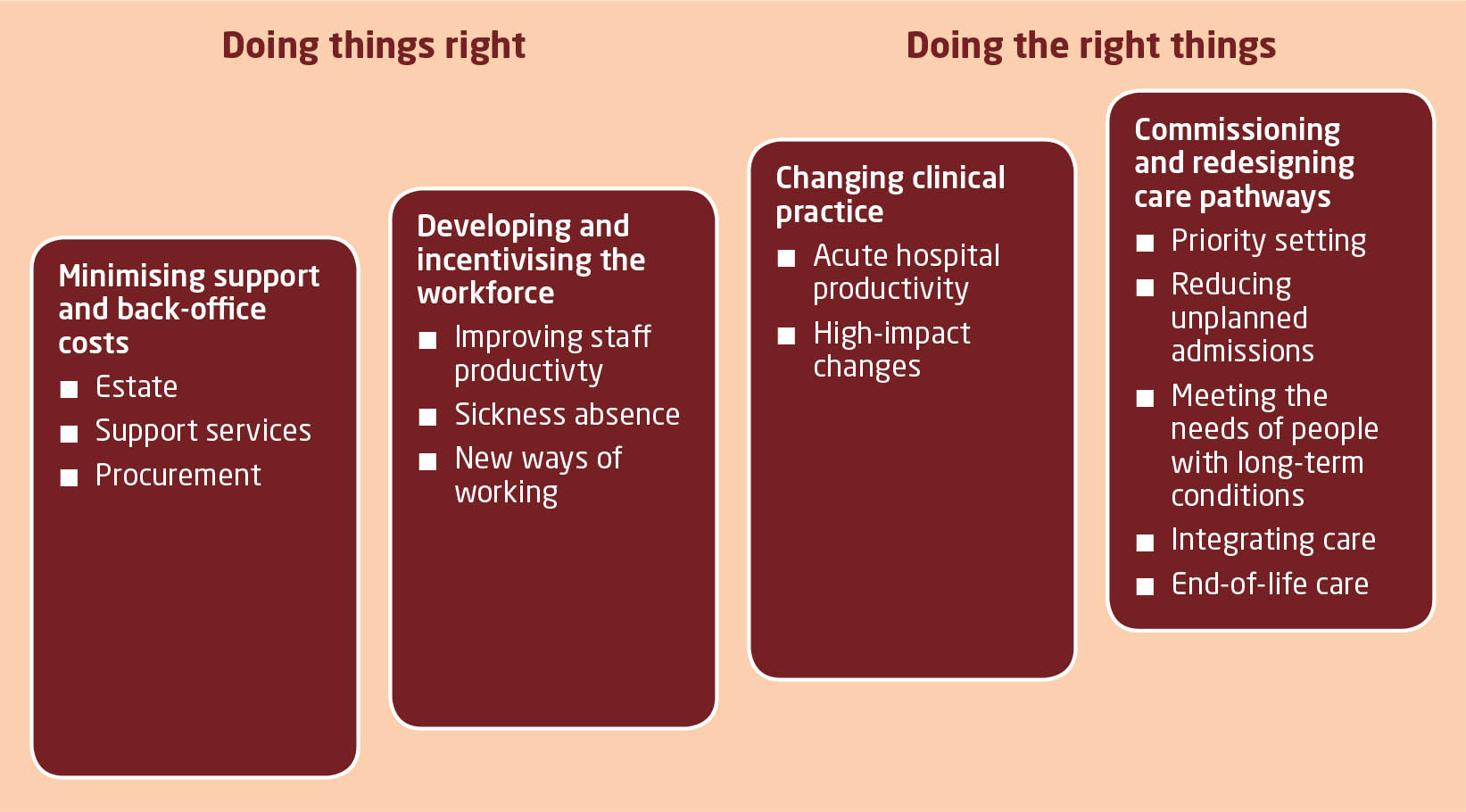
As the dementia progresses, in the later stages, a focus will be to keep the person out of hospital wherever possible. Clearly, support and care in the community need to be funded properly.
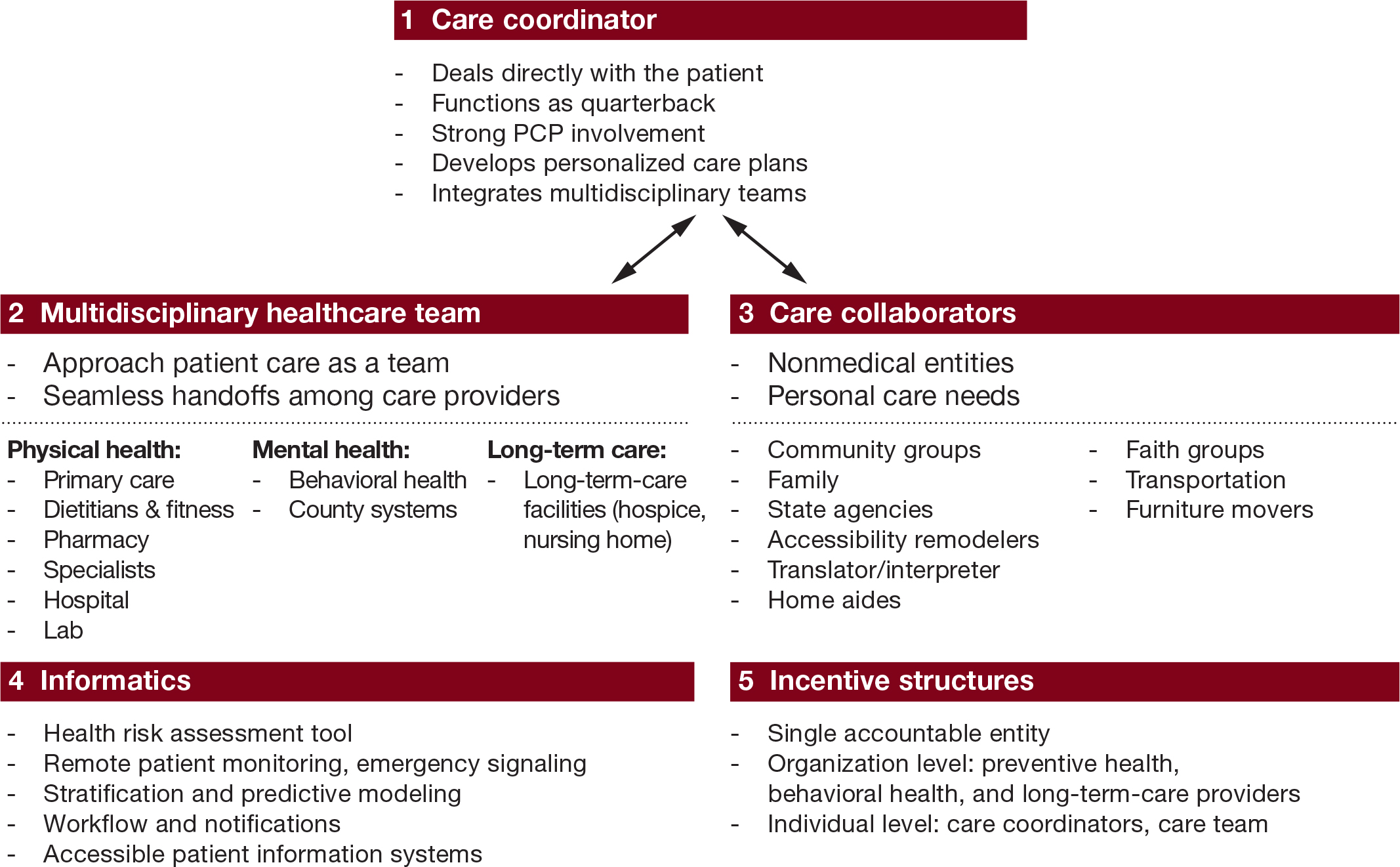
A ‘crisis’ for a person living with dementia is where a ‘stressor’ causes that person no longer to be able to cope with living in his or her usual environment. There could be a number of causes of that, but it’s noteworthy that many of them are in fact medical. I disagree a specialist nurse in dementia is necessarily a job for a community psychiatry nurse (“CPN”), as the workload of such nurses tends to be very big.
But seeing a rôle for a CPN is not a trivial one, as I’m a fully signed up devotee of ‘parity of esteem’ where mental health is not seen as the ugly sister of physical health. For that matter, social work practitioners, who often find themselves at the heart of mental capacity decisions and safeguarding issues, should be on an equal footing too with other professionals.
I said to Chris, a friend of mine living well with dementia recently, “GPs will even be in a good position to coordinate information”.
I was in fact repeating words from a GP.
Chris, “So why don’t they?”
In certain respects, in designing a system you wouldn’t wish to start from here.
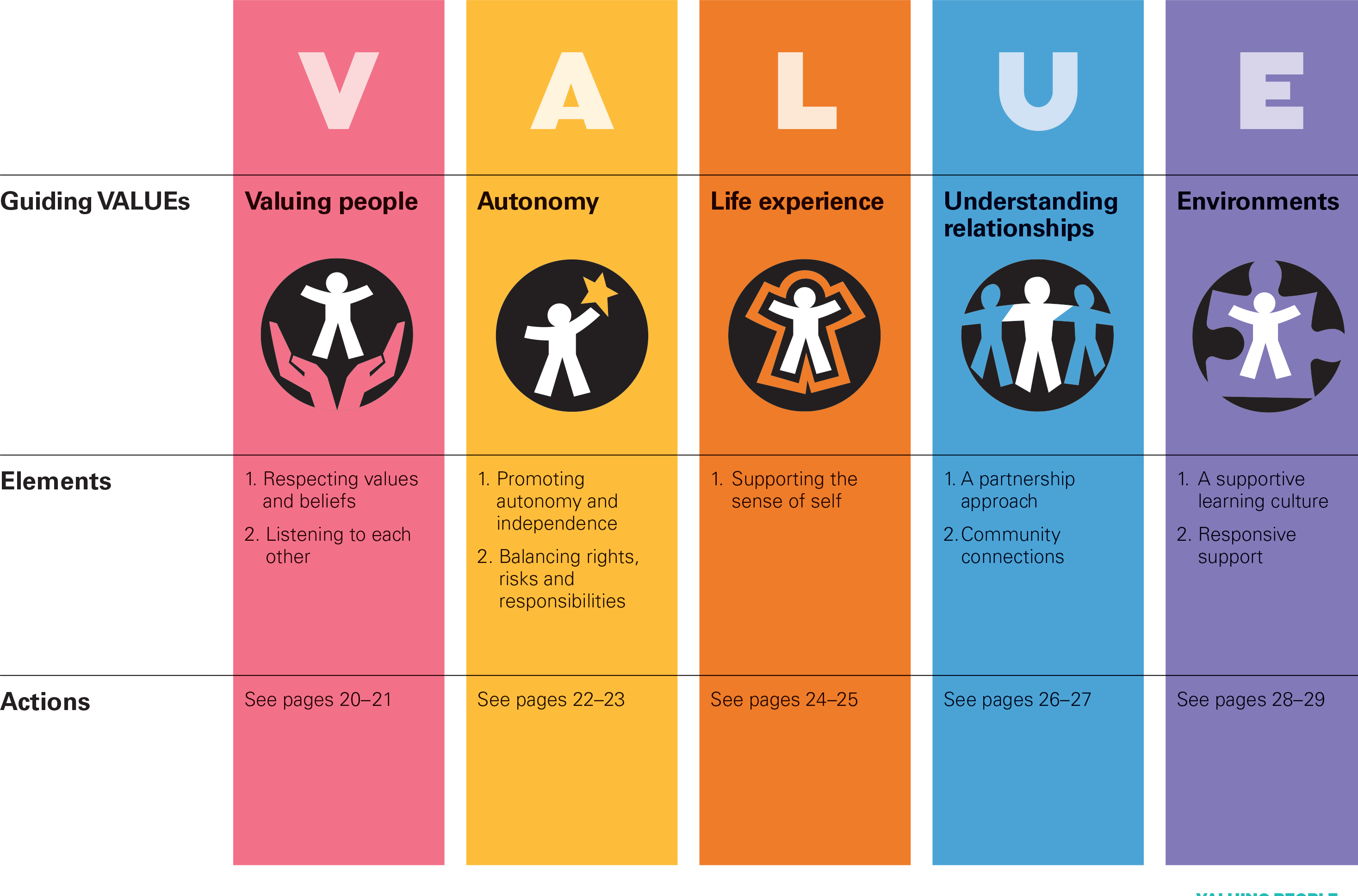
Without the focus on ‘budgets’ which do not necessarily deliver the ‘right kind’ of choice for the person with the health and care matters, it’s important that people with dementia have rights to a personal care plan, which is responsive to that person’s needs in real time. Knowing someone’s background is particularly essential in people with Alzheimer’s disease where longer term memories may be more intact. Knowing someone as a person is of course at the heart of personhood, through maybe a ‘life story’.
I don’t think it should be a ‘luxury’ of people with dementia following them after diagnosis through the system. I think, in fact, it should be an essential aspiration. It’s really important that somebody can cross off inappropriate medications, such as perhaps antipsychotics, on a drug chart if the person with dementia might not benefit.
It might help if a dementia specialist companion could spot problems in overmedicated people for blood pressure, for example. These individuals might become at risk of falls (and subsequent bone fractures if living with osteoporosis). Or somebody may be developing constipation or a stinging urine, becoming acutely confused. Dementia is not simply caused by conditions of old age, but frail individuals can do particularly bad when coming into contact with hospitals.
In the scenario that a person with dementia at any stage does need to go into hospital, it would help enormously if there could be continuity of care between the community and hospital. People with all types of dementia can find unfamiliarity, in people and environments, extremely mentally distressing, and this can be detrimental to their physical health (taking a whole person care approach). There are few people better than paid carers, with pay above the national minimum wage, and not on zero hour contracts, and unpaid caregivers including friends and family, to inform on these care plans, but the person living with dementia is the one for whom the plan is being designed.
All staff clearly need to be informed and skilled about dementia, and it is vital that resources are put aside for the adequate training of the workforce. The workforce themselves want this.
It won’t be a surprise to you to learn that I see specialist nurses in prime position to offer a huge deal to the implementation of whole person care for dementia from the next Government?
I think my views are broadly consistent with a number of places. A number of reports across jurisdictions have been important in establishing the direction of travel for acute hospital care: e.g. “Dementia care in the acute hospital setting: issues and strategies: a report for Alzheimer’s Australia” (Alzheimer’s Australia, June 2014), “Spotlight on dementia care: a Health Foundation Improvement Report” (Health Foundation, October 2011), and the Royal College of Nursing’s report “Commitment to the care of people with dementia in hospital settings” (RCN, January 2013).
Examples of appropriate clinical leads, as the RCN themselves recognise, are “Admiral nurses” from the charity @DementiaUK, Alzheimer Scotland dementia specialist nurses, dementia champions in Scotland, and ward champions. Merely having ‘dementia advisors’ will be a case of the bland and ill informed leading the bland, on the other hand.
Like many other ‘once in a lifetime opportunities’, if we get this right the service could be vastly improved. I am confident that, if given the proper funding to make this happen, and strong leadership cascades downwards, the next Government will rise to this challenge.