In my rather extremist world, I believe all dementia and delirium care should be person-centred. In other words, I don’t care much for the notion that donepezil and memantine ‘work’ on chemical receptors, regardless of one’s sex, ethnicity, and so on. Like many people, as a son of a wonderful mum with dementia, I don’t like the term ‘lived experience’ because it is a term patently invented for the purposes of fundraising and conferences. I think the term ‘engagement’ is utterly fraudulent, because people are rarely ‘engaged’ on equal terms such that both parties benefit to equal extents. And I’ve seen with my own eyes how aspects of dementia policy, including dementia friendly communities, can become a sketchy fig-leaf for marketing purposes; a form of ‘diversity marketing’ or provision of an ‘unique selling point’.
You can come at whether services should be uniquely provided for a particular group, such as Asian people, or people with young onset dementia, in a similar way to whether geriatricians should providing an unique service for older people. For example, you wouldn’t necessarily think that all people in Ireland are the same, and therefore have the same needs. This has its roots in deep seated problems. Think about whether people with dementia have enough in common for you to suggest the notion of ‘dementia friendly communities’, when arguably ‘friendly communities’ should be ‘friendly’ to all. This demands an answer to the question whether the groups of people you define have sufficiently in common, such as ‘young onset dementia’, for them to be considered in a separate segregated group, other than the marketing justification of ‘unique selling point’. The problem with considering ethnic groups separately, for example, is that we end up segregating people further, encouraging a sense of ‘otherness’, when what we want to be encouraging are services or a community inclusive of all.
In my experience, as a son, who is Asian, I think it’s great that carers can be person-centred, but this does not simply stop at being of the same sex, or same ethnic background, or same religion. Respecting sociocultural differences has to be thought about from the practicalities of caring too. For example, an older woman who is muslim with advanced dementia might feel unnecessarily distressed at having somebody changing her incontinence pad who is male and speaks a different language. I found this recently when a befriending partner proposed for mum, with the same sex and same country of origin, could not form a relationship with mum because they spoke entirely different dialects of Bangladeshi.
If you don’t get bogged down in diversity marketing, it is easy to get overwhelmed in equity of access to services for people from particular groups, e.g. LBGT, BAME, etc. But you can’t half observe person-centred care. You have to treat each person’s individuality, even if you group them according to a characteristic. And my conclusion is that too much is over claimed about people with cognitive disabilities being treated to their detriment under equality legislation. The number of successful cases taken under the protected characteristic of dementia (under disability) is insufficient to draw any meaningful conclusions, and the general situation over legal aid means that people are hard pushed to take up legal claims anyway.
The assessments of cognitive function have to be culturally fair. Just as in assessing mental capacity you should allow for language differences or sensory impairments (e.g. deafness), it is essential that some accommodation is made for cultural backgrounds of people presented as perhaps having dementia. We tend to make other assumptions about all people from all sociocultural backgrounds, as regards their network of friends and family, even when considering broad groups of people such as ‘women’. Even if you exclude one person, that, in my opinion, is a failure. It’s no good saying you have an outreach of 95%, if the other 5% are off the RADAR. And please try not to use that over-used word from the conference and corporate circuit, “hard to reach”. Again, I think the critical thing is not getting in touch with people with dementia and carers ‘for the sake of it’. You have to ask yourself – why have they disappeared off the RADAR? Is it something as simple as the fact that dementia charities sell their products to a particular social clique, and are largely represented by activists and advocates from a particular social clique? Or is that they don’t all use smartphone apps?
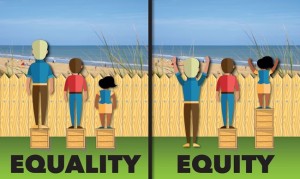
Equity is not necessarily the same as equality.
It’d impossible to escape from a need to consider what the factors are which cause some people to be over-represented rather than others, and this has to include a consideration of the factors which make us healthy (e.g. determinants such as housing, money, transport). But this applies to everyone – not just people in particular sociocultural backgrounds. The problem with taking the ‘equality ‘ approach, that groups of people have particular disabilities, and need help to get them up to the same level, is that you all too easily abolish diversity. The clue is in the name ‘dementia friendly communities’ which treats people with dementia (similarly to carers) as one huge homogeneous mass.
All too often the mentality has been tick-boxy in being seen to provide ‘equality and diversity’, without thinking through any of the issues or how they relate to each other. A charity which is fundraising may want to present an image that ‘nobody is left behind’, particularly if a person might donate money or contribute to a research project, but it is an altogether different ethos to embrace genuine inclusivity’ ‘nothing about us without all of us’, and really really mean it.